Intensivist
A Valued Resource for Pediatric Intensivists
Insights to Improve Critical Care Quality & Outcomes in Your Unit
What We Do
VPS, LLC brings together a community of pediatric critical care colleagues who are dedicated to standardized data sharing, benchmarking, quality improvement and research among pediatric ICUs to improve the care of their patients.
Participants commit to the collection of high-quality data elements that are important to understand, evaluate and improve care and outcomes for critically ill children using comparable and customizable reports and dashboards.
The VPS Community collaborates to compare data, determine best practices and improve the overall quality of pediatric critical care.
A Valued Resource for Pediatric Intensivists
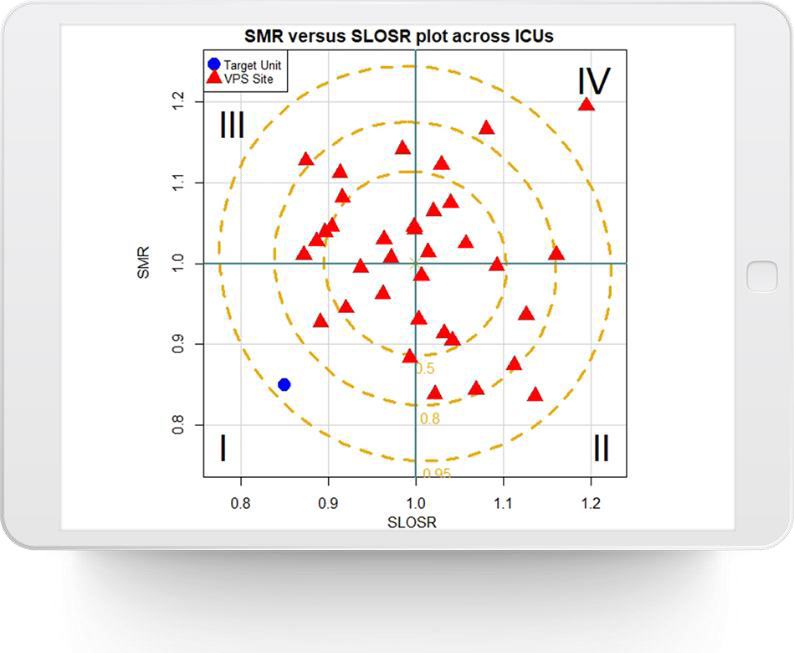
VPS is the Only Way to Truly Benchmark Your PICU’s Performance as a
Fundamental Requirement for Quality Improvement
Quality
Understand the Current State of Your PICU and Improve Quality, Safety and Efficiency with Valid, Comprehensive Clinical Data
Case Study: Kaiser Northern California presents their discharge delay data, with estimated cost savings, during senior leadership meetings.
Case Study: Children’s Medical Center Dallas uses the quarterly mortality data to monitor for spikes that prompt them to dive deeper into M&M reviews. These deeper dives have led them to initiate improvement projects to correct issues.
Case Study: Akron Children’s Hospital uses VPS data to standardize reporting for CLABSI and CAUTI. VPS allows them to develop severity-adjusted local rates and exploring acuity-adjusted prevention/interventions.
Access Data for National Improvement Collaboratives Such as Solutions for Patient Safety (“SPS”)
Administrative
Benchmark Against Other Units Throughout the Country to Compare Outcomes and Case Mix
Case Study: Children’s Medical Center Dallas uses VPS data to follow activity over time in comparison to peers. They use reports to share the data with their Quality Committee.
Use Trend Data to Justify Requests for Additional Staff
Case Study: Texas Children’s Hospital used VPS data to help justify the expansion of 32 PICU beds to 84 PICU beds. The unit established cohorts by using the VPS data (diagnoses, star codes, etc.) to determine how many PICU beds were needed by specialty.
Identify Opportunities for Missed Billings
Case Study: Rainbow Babies and Children’s Hospital uses VPS to create a list of all patient days that should have generated a bill in order to double check their billing records and ensure no lost revenue.
Research
Leverage a Rich Source of Multi-Institutional Data for Clinical Research Including AHRQ, PALISI and AAP
VPS has an active research community with more than 100 active research studies underway from over 35 participating children’s hospitals.
Over 200 scientific publications have used VPS data in high-impact peer reviewed journals.
Five Calibrated Models for Morbidity and Mortality Prediction (PIM3, PRISM III, PRISM IV, PICSIM, And PELOD) to Assess Severity of Illness and Organ Dysfunction
New-morbidity functional status is an intermediate outcome towards mortality in the PICU. Knowledge of the morbidity status of a patient allows prevention of secondary injuries and to preserve function. Functional Status Score (FSS) and the PCOP/PCPC are available to assess morbidity.
Customizable & Comprehensive Reports
Provide clinicians and administrators with:
- Support for key initiatives: quality improvement, outcomes enhancement, accreditation (Joint Commission, Leapfrog), board and community level administrative reports, clinical transformation, budgeting and strategic planning.
- Administration-level reports uniquely packaged and customizable for review by hospital administration and Board of Directors.
- Case Study: Helen DeVos Hospital developed timely, effective responses to novel challenges (e.g. COVID-19) with accurate, real-time national data.



The VPS Difference
Only Pediatric ICU Database Using Validated Severity of Illness Scores (PIM3, PRISM III, PRISM IV, PICSIM, and STS-EACTS)

What Clinicians Are Saying
VPS has been an invaluable and essential resource to support and drive clinical, operational, quality improvement, and research initiatives in both the Pediatric Intensive Care Unit and throughout the
hospital. This timely granular data has provided powerful support, directly impacting patient care
quality and outcomes.

Akira Nishisaki, MD, MSCE
Attending Physician, Critical Care Medicine,
Children’s Hospital of Philadelphia

Steven L. Shein, MD
Rainbow Babies and Children’s Hospital

Michael L Forbes, MD, FCCM, FAAP
Akron Children’s Hospital